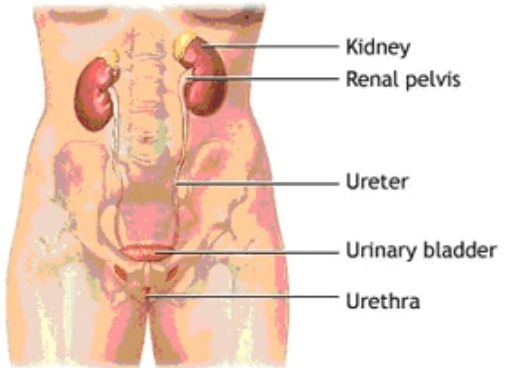
The urinary tract is made up of the kidneys, the ureters, the bladder, and the urethra.
Kidneys
The kidneys are a pair of bean-shaped organs located near the middle of the back. Each kidney filters waste products from the blood to form urine. Urine collects in tubules that eventually drain into the renal pelvis which continues as the ureter.
Ureters
The ureters are tubes that convey the urine from the kidney to the bladder. Muscles in the ureter walls constantly tighten and relax to force urine downward away from the kidneys. If this passage is blocked by a stone or by disease, kidney infection can develop. The area where the ureters enter the bladder is called the trigone. Valves in this region prevent the backing up of urine (reflux) into the kidneys.
Bladder
The urinary bladder is a hollow, muscular balloon that stores urine from the kidneys until it is an appropriate time to void. The bladder narrows down to an opening called the bladder neck. The bladder neck is surrounded by muscles called the internal sphincter which tighten around the urethra to prevent urine from leaking as the bladder fills. The bladder expels urine out of the body via the urethra.
Nerves in the bladder tell you when it is time to empty your bladder. When the volume of urine in the bladder reaches a certain capacity, the brain sends impulses to the internal sphincter to relax and to the bladder wall muscles to contract and expel urine. When all the signals occur in the correct order, normal urination occurs The bladder can usually hold up to 300-400ml of urine comfortably for 2-5 hours. Most people pass urine about 6-8 times a day.
Urethra and urethral sphincters
The urethra is the tube that passes urine from the bladder out of the body. The female urethra starts at the bladder neck and exits the body directly in front of the vaginal opening.
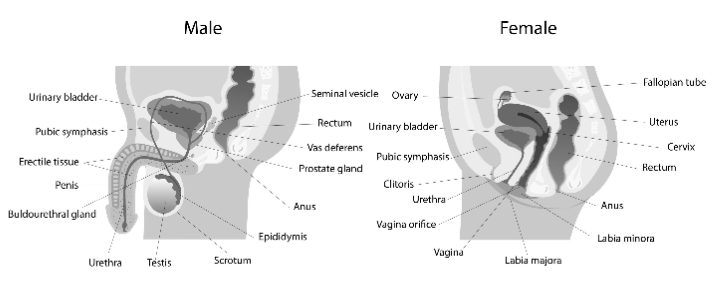
In men, the urethra is roughly 8 to 9 inches long and extends from the bladder neck to the end of the penis. The male urethra is composed of three parts: prostatic, membranous, and spongy. The prostatic urethra is the widest part of the tube and passes through the prostate gland.
Circular muscles called the external urethral sphincter also help keep urine from leaking. The sphincter muscles close tightly like a rubber band around the opening of the bladder into the urethra. This sphincter re-inforces the internal sphincter and is under voluntary control. This is one of the parts you learn to strengthen when you are taught pelvic floor exercises.
Male Reproductive System
The male reproductive system is made up of the penis, testicles, epididymes, vas deferens, prostate, and seminal vesicles.
Penis
The internal structure of the penis consists of two spongy cylinder-shaped bodies (corpora cavernosa) and the urethra (tube for expelling urine and ejaculate). Blood fills the spongy tissue to form an erection.
Testes
The testes are responsible for producing sperms and testosterone. Each testis is connected to a small, coiled tube called the epididymis, where sperm are stored for as long as 6 weeks while they mature.
The epididymes are connected to the prostate gland by a pair of tubes called the vas deferens. This transports the sperms to the urethra and is the part that is tied up in a vasectomy.
Prostate Gland
The prostate is a ping pong ball-sized gland located beneath the bladder and in front of the rectum. It produces the milky fluid that combines with sperms to become semen. The urethra (tube that transports urine and semen out of the body) passes through it.
Seminal Vesicles
The seminal vesicles are 2 little sacs located just behind the prostate. They store and secrete a thick fluid that mixes with seminal fluid produced by the prostate and sperm from the testes to form semen.
Female lower urinary tract
The female bladder lies in front of the uterus (womb) and behind the pubic bone. The female bladder, bladder neck and urethra is supported by the pelvic muscles at the base like a hammock. Disruption, damage or loss of strength at this hammock can lead to pelvic organ prolapse and /or stress incontinence.